Clinical information for General Practitioners in Newcastle and the Hunter Region
(Evidence-based summary adapted from RANZCP Clinical Guidelines & NEDC GP Resource)
Managing Eating Disorders in
Primary Care - GP Quick Guide
Eating disorders carry serious medical risk and are not primarily psychiatric presentations; they are medical illnesses with psychological features. Early GP involvement improves safety, reduces risk of hospitalisation, and supports coordinated care.
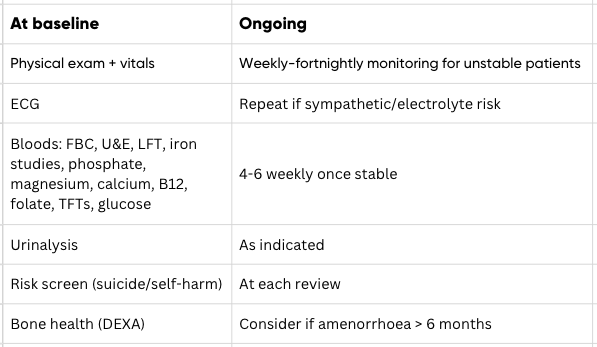
Recommended GP monitoring
RED FLAGS: Consider same-day review or hospital assessment if any of the following indicators are present (RANZCP)
Eating Disorder Plan (EDP) – MBS (recommended when criteria met)
Patients may access:
Up to 40 psychological sessions (CBT-E, FBT, SSCM etc.) with Psychiatrist review at 20 sessions
Up to 20 dietetic sessions
Requires EDE-Q global score > 3 (not required for anorexia nervosa)
Must demonstrate functional impairment or medical risk
Requires GP review at 10, 20, 30 sessions
Mental Health Care Plan (MHCP)
Use when EDP criteria not yet met or diagnosis unclear.
Chronic Disease Management Plan (CDM)
May be used alongside EDP for medical conditions.
Medicare pathways for treatment
Effective treatment requires team-based management:
GP – medical monitoring + care plan
Psychologist – eating disorder treatment
Dietitian – meal structure & weight restoration
Family/carer involvement when appropriate
Referral to higher-level care if risk escalates
Multidisciplinary care
Refer to an eating disorder–informed psychologist where:
Restrictive eating, binge–purge behaviours, compulsive exercise
Body image disturbance or significant weight concern
Weight loss, medical instability, or fasting behaviours
Emotional dysregulation/anxiety/depression with disordered eating
When to refer to a psychologist
Hunter New England Health – Eating Disorder Services (via GP referral), including day program (James Fletcher) and residential treatment (REDC)
ANZAED Credentialed Provider Directory – https://connected.anzaed.org.au
InsideOut Institute – EDP templates & tools https://insideoutinstitute.org.au
Local pathways in Newcastle & The Hunter
At Life Matters Psychologists, we provide eating disorder–informed psychological treatment for adolescents and adults across the Hunter region, using evidence-based therapies (CBT-E, SSCM, ACT and FBT principles).
Led by clinical psychologist and director, Matthew Stanton, and clinical psychologist and ED specialist, Sinead Day, we work collaboratively with GPs and dietitians and support safe shared care plans.